Periodontitis is an advanced form of gum disease that is caused by a bacterial infection of the soft tissues surrounding the teeth. It can affect anyone with poor oral hygiene who fails to brush and floss regularly and can lead to tooth loss if left untreated. Periodontitis affects more than 47 percent of U.S. adults over the age of 30, and 70 percent of adults aged 65 and older.
A history of gum disease in the family can increase the likelihood of developing periodontitis. Other risk factors include smoking, diabetes, hormonal changes due to pregnancy or birth control pills, and health conditions associated with inflammation, such as arthritis and cardiovascular disease.
Stages of Periodontitis
Periodontitis is a progressive disease, meaning it advances to more serious levels when ignored.
There are four stages of periodontitis:
- Gingivitis – The earliest stage of the disease, the hallmark of gingivitis is red and swollen gums. Other symptoms include gums that bleed easily, especially when brushing, and sensitivity to hot or cold foods. You are not at risk of tooth loss at this stage, with gingivitis being reversible with proper oral care and regular cleanings with your dentist.
- Mild periodontitis – Periodontitis begins to set in when gingivitis is not addressed, with the gums beginning to pull away from the teeth and periodontal pockets beginning to form. This allows plaque, tarter, and bacteria to become easily lodged in those pockets, exacerbating the issue since neither a toothbrush nor floss can reach these spaces.
- Moderate periodontitis – Bone loss around the teeth progresses, and bacteria continue to erode the soft tissue that keeps your teeth healthy and in place. Mild pain, including sore and tender gums, is common at this stage. Moderate periodontal disease is usually identified by a dentist measuring the pockets around the teeth.
- Severe periodontitis – At this stage, teeth begin to loosen and fall out. Bleeding gums are common, and infections along the gum line can lead to other oral health issues such as halitosis. Severe periodontitis can also start to impact overall health when the bacterial infection travels to the bloodstream, leaving you susceptible to heart disease, stroke, and other serious health complications.

Symptoms of Periodontitis
Periodontitis is an oral health disease that is commonly ignored despite plenty of symptoms pointing to an escalating problem. Healthy gums fit tight around each tooth and are firm to the touch; therefore, anything that deviates from this should be addressed with your dentist.
Signs of periodontitis include:
- Red or purple gums, instead of the usual pink
- Swollen or tender gums
- Gums that bleed easily
- Bad breath
- Visible infection around the gumline
- Loose teeth or tooth loss
- Gum recession
- Painful chewing
- New spaces between teeth
In order to diagnose periodontitis, a dentist will perform a visual examination to identify any signs of gum inflammation. They will then use a periodontal probe, which resembles a small ruler, to measure any pockets around your teeth. Dental X-rays may be taken to check for bone loss, and more advanced cases may be referred to a gum disease specialist, known as a periodontist.
Periodontitis Treatment
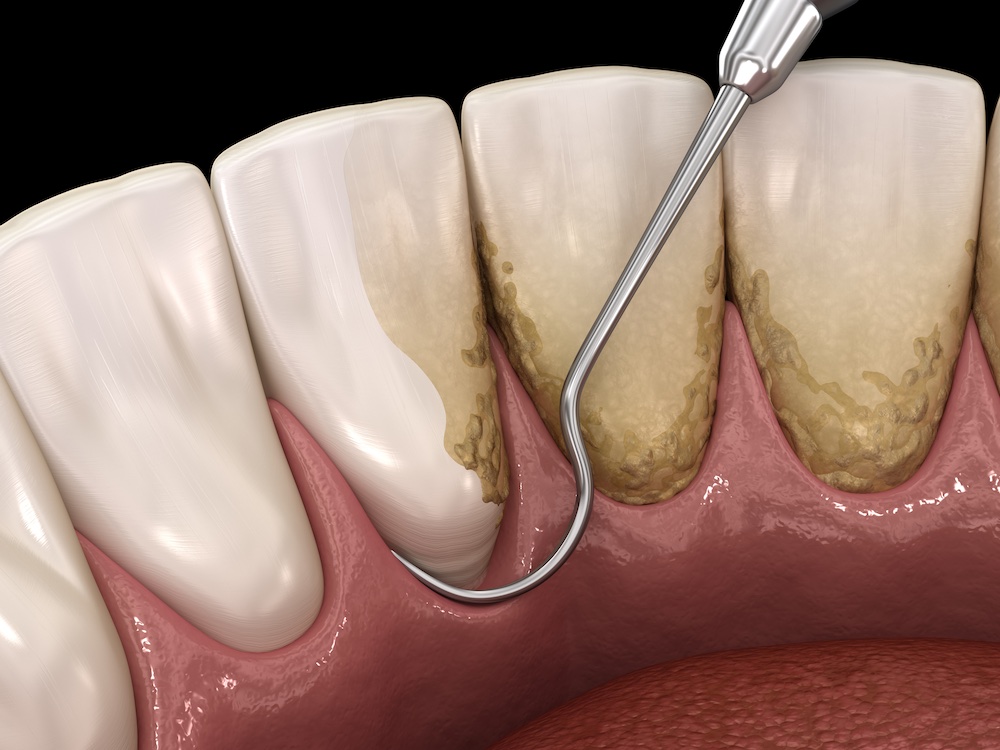
Depending on the stage of periodontitis, a few treatment options are available. Your dentist can perform scaling and root planing, which involves a deep cleaning of the teeth and gums to remove plaque, tartar, and bacteria from the entire gum line area. This is only helpful in the earlier stages of the disease. For moderate and severe cases, pocket reduction surgery, which is a surgical procedure to access and clean the pockets to avoid further progression, might be recommended. This involves gently lifting the gum tissue, cleaning the underlying area, and stitching the gum tissue back into place.
If you have any additional questions about periodontitis and its various stages, contact us.